Neoadjuvant immunotherapy in mismatch-repair-proficient colon cancers
Article Meta
Article Date: 20 October 2025
Article URL: https://www.nature.com/articles/s41586-025-09679-4
Article Image: Image
Summary
This Phase II NICHE study reports neoadjuvant nivolumab plus ipilimumab in 31 patients with early-stage mismatch-repair-proficient (pMMR) colon cancer. The overall pathological response rate was 26%, including six major pathological responses (≤10% residual viable tumour), and one patient achieved an ongoing clinical complete response and did not undergo surgery. Circulating tumour DNA (ctDNA) was detectable in most patients at baseline (26/31); ctDNA clearance before surgery occurred in 5 of 6 responders but in only 1 of 20 non-responders. Responding tumours had low tumour mutational burden but higher chromosomal genomic instability scores, greater expression of proliferation signatures and TCF1, and more Ki-67+ cancer cells and Ki-67+ CD8+ T cells on imaging mass cytometry. The paper identifies candidate biomarkers that may help select pMMR colon cancers likely to benefit from neoadjuvant immune checkpoint blockade (ICB).
Key Points
- Neoadjuvant nivolumab + ipilimumab produced a 26% response rate in early-stage pMMR colon cancer (6 major pathological responses, 1 clinical complete response).
- ctDNA was positive in most patients at baseline; clearance correlated strongly with responders (5/6 cleared before surgery) versus non-responders (19/20 remained ctDNA+).
- Responses occurred despite uniformly low tumour mutational burden, indicating TMB alone is not predictive in this setting.
- Higher chromosomal genomic instability scores associated with response, suggesting genomic instability may identify responsive tumours.
- Responding tumours had higher proliferation signatures, higher TCF1 expression and increased Ki-67+ tumour and CD8+ T-cell populations, pointing to immune–tumour proliferative interactions as potential biomarkers.
- The study offers a multi-modal biomarker set (ctDNA dynamics, genomic instability, proliferation/TCF1, Ki-67+ immune contexture) to improve patient selection for neoadjuvant ICB in pMMR disease.
Content summary
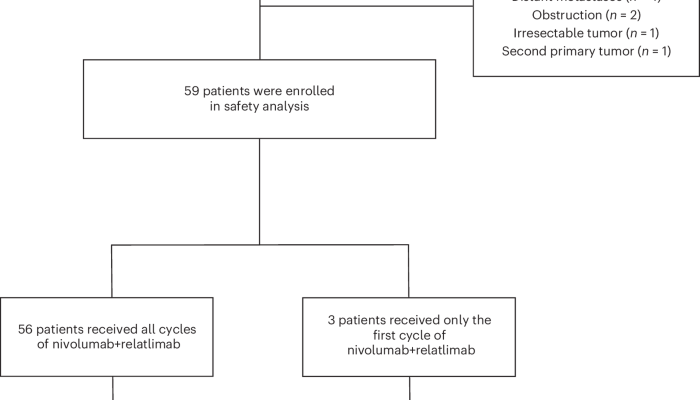
The NICHE phase II trial enrolled 31 patients with early-stage pMMR colon cancer who received a short course of combined anti-PD-1 (nivolumab) and anti-CTLA-4 (ipilimumab) therapy before planned surgery. Pathological assessment post-treatment showed meaningful responses in a subset, including major pathological responses. The investigators performed integrated analyses: ctDNA monitoring, tumour sequencing to measure tumour mutational burden and chromosomal instability, transcriptomic signatures for proliferation and TCF1, and high-plex imaging mass cytometry to quantify proliferating cancer cells and proliferating CD8+ T cells. ctDNA clearance correlated with response and could be an early on-treatment indicator. Importantly, responders were not defined by high TMB but by higher chromosomal instability and a proliferative, TCF1-high tumour microenvironment with active proliferating CD8+ T cells.
The authors propose that combining ctDNA dynamics with tumour genomic and immune phenotypes may identify pMMR colon cancer patients who can benefit from neoadjuvant ICB and support further prospective validation.
Context and relevance
ICB has been transformative in several cancers but has had limited success in metastatic pMMR colorectal cancer. This study shifts focus to early-stage disease and neoadjuvant use, showing that a subset of pMMR tumours can respond when treated preoperatively. The work is relevant to clinicians and researchers interested in expanding immunotherapy indications, improving patient selection with biomarkers, and integrating ctDNA into clinical decision-making. It aligns with trends toward personalised perioperative oncology and combining multi-omic biomarkers to predict immunotherapy benefit.
Why should I read this?
Short answer: because it punches a hole through the idea that pMMR colon cancers never respond to checkpoint inhibitors. If you care about making immunotherapy work for more patients, this paper gives you visible clues — ctDNA clearance, chromosomal instability and a proliferative/TCF1-high immune environment — that help pick winners. We read the long methods and dense figures so you don’t have to; this is a useful snapshot if you’re thinking about trials, biomarker panels or perioperative treatment changes.