Hepatic zonation determines tumorigenic potential of mutant β-catenin
Summary
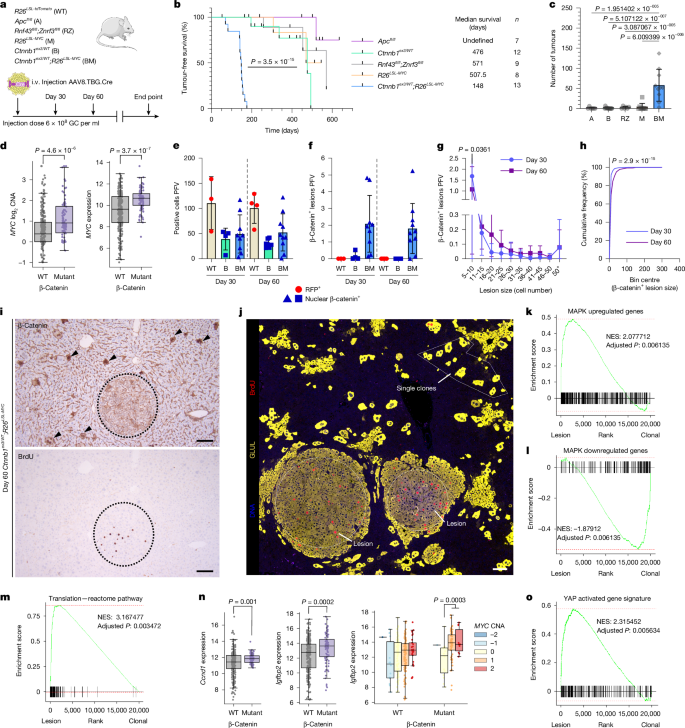
Published: 19 November 2025 — Raven et al. use sophisticated mouse mosaics, spatial transcriptomics and ribosome profiling to show that the liver’s zonal architecture determines whether hepatocytes bearing oncogenic β-catenin (CTNNB1) mutations will form tumours. The homeostatic WNT gradient drives zone 3 (pericentral) differentiation (GLUL+/Lgr5+). Paradoxically, this zone 3 differentiated state resists tumour formation: mutant β-catenin must avoid or reverse a strong zone-3 fate and engage a zone-2-like IGFBP2–mTOR–CCND1 pro-growth programme to expand.
Key experimental findings: sporadic CTNNB1 exon-3 mutations are weakly oncogenic unless paired with elevated MYC; proliferative lesions show reduced nuclear β-catenin and activation of MAPK, mTOR and translation programmes; GLUL+ (zone 3/Lgr5+) hepatocytes are refractory to WNT-driven proliferation; activating MAPK (BRAF V600E) can antagonise zone-3 differentiation and unlock tumorigenesis in central-vein hepatocytes; by contrast, strong WNT activation via APC loss is less permissive to tumour growth. Pharmacological inhibition (rapamycin, PORCN or BRAF inhibitors) modulates lesion formation and established tumour growth in the models used.
Key Points
- Zonation matters: the liver’s WNT gradient forces zone-3 differentiation that is not permissive to oncogenic expansion of β-catenin-mutant hepatocytes.
- CTNNB1 exon-3 point mutations are common in HCC and often co-occur with MYC copy gain; MYC elevation enables tumour progression in mouse mosaics.
- Early proliferative lesions show reduced nuclear β-catenin but increased MAPK, mTOR signalling and a pro-growth translatome (increased translation efficiency of growth-related mRNAs).
- IGFBP2–mTOR–CCND1 axis (a zone-2 programme) is required for oncogenic expansion; disrupting IGFBP2 or transient mTOR inhibition (rapamycin) reduces lesion formation and later tumour burden.
- GLUL+ (Lgr5+) zone-3 hepatocytes resist WNT-driven tumour initiation; converting their fate (via MAPK/BRAF activation) suppresses zone-3 differentiation and enables tumourigenesis.
- APC loss (stronger, uniform WNT activation) produces intense nuclear β-catenin but is less tumourigenic than CTNNB1 exon-3 mutations in these liver models.
- Therapeutic implication: targeting mTOR, WNT-ligand secretion (PORCN) or MAPK (BRAF) can suppress tumour growth in relevant genetic contexts.
Why should I read this?
Quick — read this if you want to stop thinking of WNT as a simple on/off cancer switch. The paper shows that where a hepatocyte sits in the lobule (and what differentiation programme it adopts) determines whether a β-catenin mutation is dangerous. It also points to real druggable vulnerabilities (mTOR, PORCN, BRAF) and explains why CTNNB1 exon-3 hits are selected in HCC. If you work on liver cancer, zonation, or WNT biology, this is proper must-read stuff.
Context and relevance
Why it matters: this work reframes oncogenic WNT signalling in the liver as a context-dependent process — ‘just right’ WNT activity and the cell’s zonal fate together control tumour initiation and progression. It explains clinical observations (prevalence of CTNNB1 hotspot mutations, frequent MYC co-amplification) and highlights that tumourigenesis requires both dampening of a zone-3 differentiation programme and engagement of a pro-growth translational programme. The findings link zonal homeostasis, regeneration and cancer initiation and open up strategic intervention points for chemoprevention or early treatment (for example, transient mTOR targeting to block early lesion expansion).