Prevalence of Alzheimer’s disease pathology in the community
Article meta
Article Date: 17 December 2025
Article URL: https://www.nature.com/articles/s41586-025-09841-y
Article Image: Figure 1
Summary
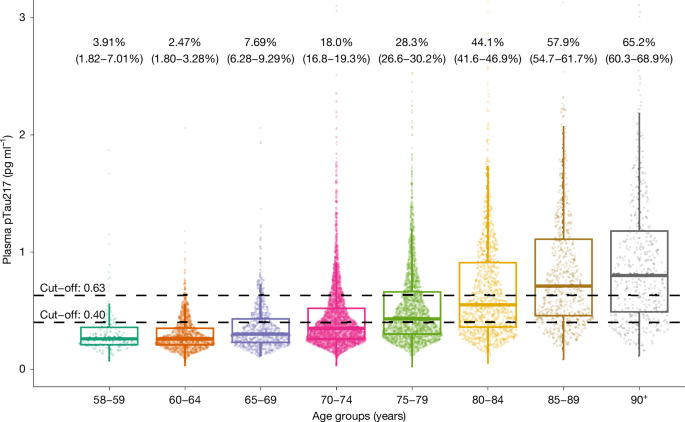
This large, population-based Norwegian study measured plasma phosphorylated tau at threonine 217 (pTau217) in 11,486 samples from people aged 58 and older (HUNT3 and HUNT4 cohorts) to estimate the prevalence of Alzheimer’s disease neuropathological changes (ADNCs) in the community. Using validated cut-offs (rule-out <0.40 pg ml−1; rule-in ≥0.63 pg ml−1), the authors found that prevalence rises sharply with age: under 8% in ages 58–69.9, 33.4% in the 70+ group and 65.2% in those aged 90+. In the 70+ population, estimated prevalence breakdown was 10% preclinical AD, 10.4% prodromal AD and 9.8% AD dementia.
Plasma pTau217 positivity correlated with APOE ε4 allele count and lower education, and showed an inverse relationship with kidney function below an eGFR threshold. Approximately 11% of people aged 70+ would meet current eligibility criteria for disease-modifying therapies (DMTs) against amyloid. The study highlights an intermediate biomarker zone (0.40–0.63 pg ml−1) affecting 13.5–27.6% of participants and discusses implications for follow-up testing, treatment planning and service demand. Limitations include cross-sectional design, a predominantly white Norwegian population and self-reported comorbidities.
Key Points
- Sample: 11,486 plasma samples from the HUNT population study (58+ years).
- Biomarker: plasma pTau217 measured with validated ALZpath p-Tau 217 assay; two cut-off approach used to define negative, intermediate and positive ADNC status.
- Age trends: ADNC prevalence rises from <8% (58–69.9 years) to 65.2% in people >90 years; 33.4% in the 70+ group overall.
- Clinical groups (70+): 10% preclinical AD, 10.4% prodromal AD (MCI), 9.8% AD dementia; 60% of people with dementia had biomarker-verified ADNCs.
- Treatment eligibility: about 10.2% of measured 70+ participants (weighted estimate 11.1%) met current DMT eligibility criteria.
- Risk modifiers: higher prevalence with one (46.4%) or two (64.6%) APOE ε4 alleles; higher prevalence with lower education; inverse association with eGFR <~51 ml/min/1.73 m2.
- Intermediate zone: 13.5–27.6% had intermediate pTau217 values and would need further testing or repeat measures.
- Limitations: cross-sectional design, selection/participation bias adjusted by weighting, predominantly white Norwegian cohort, self-reported comorbidities.
Context and relevance
This is the largest population-based estimate to date using a blood-based pTau217 marker. As anti-amyloid/immunotherapy options expand, reliable prevalence data are vital for healthcare planning, estimating numbers eligible for DMTs and forecasting resource needs (diagnostic work-up, infusion services, imaging and monitoring). The work demonstrates how scalable blood biomarkers can reframe estimates of who truly has AD pathology in the community — not just who has cognitive symptoms — and refines expectations about treatment demand in older age groups.
Why should I read this?
Short version: if you care about how many people actually carry Alzheimer’s pathology (and who might be eligible for new treatments), this paper is gold. It uses a big community sample and a validated blood test to give much clearer, age-stratified estimates — so you don’t have to wade through small clinic studies or guesswork. Handy for clinicians, service planners and policy folk who need real-world numbers fast.
Source
Source: Prevalence of Alzheimer’s disease pathology in the community — Nature (17 Dec 2025)